The lunacy of the low-fat craze has taught most Paleo dieters to look at public health campaigns with a healthy dose of skepticism. We don’t blindly accept established medical wisdom just because the doctor said so, or reflexively adjust our diet to every new recommendation that comes along. But that doesn’t mean that the medical establishment is always wrong – and the campaign to reduce sodium seems to be one of its potentially useful recommendations. After all, if the average sodium intake in the Paleolithic was 768 mg, and the average American consumes 3,436 mg per day, couldn’t excessive salt intake be another harmful part of the modern diet? It sounds logical, but governmental recommendations for sodium restriction are actually based on seriously flawed data and have the potential to do much more harm than good.
Sodium Basics
Sodium is a naturally-occurring element found in everything from milk to beets to celery sticks. Most people’s main source of dietary sodium is table salt (sodium chloride), which is 40% sodium; fancier sea salts contain roughly the same amount of sodium, although they also contain several other trace minerals that are stripped from table salt during processing. Sodium is crucial for maintaining proper muscle and nerve function and electrolyte balance. It helps maintain the volume of blood plasma, an important balance for heart health. Salt also aids in digestion by providing chloride to the hydrochloric acid (HCL) in your stomach.
The body processes salt and maintains body fluid homeostasis primarily through a system called the RAAS (renin-angiotensin-aldosterone hormonal system). The kidney is the primary organ involved – and in a healthy adult, it can adapt without a problem to a wide variety of dietary salt levels. If you eat a large amount of salt, your kidneys excrete more sodium, to reduce your blood plasma volume to normal levels. If you eat very little salt, your body produces more of two hormones called renin and aldosterone, causing you to retain more sodium and maintain adequate fluid balance and blood pressure. While renin can help regulate your sodium levels, chronically high renin levels are inflammatory.
We lose salt every day through urination and sweating, and the human body has no way of synthesizing sodium from other dietary elements, so some salt consumption is clearly necessary. The specific amount, however, is much less clear.
The INTERSALT Study
Citing a correlation between sodium intake and high blood pressure, public health officials constantly encourage Americans to reduce our consumption of salt. But salt wasn’t always this demonized. Throughout history, humans have sought it out, prized it – and, until very recently, preserved most of our food with it. The modern salt phobia started in 1972, when a study done on genetically hypertensive rats claimed to show that dietary sodium produced hypertension, while dietary potassium reduced it. The rats in this study, however, consumed an amount of sodium completely outside the realm of plausibility for anyone with a choice in the matter. To reach the same level of sodium intake relative to his body weight, a human would have to eat over 500 grams of sodium – compared to an average intake of around 3.5 grams a day in the US. To get 500 grams of sodium, you’d have to eat 4.5 cups of table salt. Anything would be harmful in such extreme amounts, even water. This study proves nothing about the effects of sodium consumption at a level that anyone but a force-fed lab rat would eat.
The 1972 study started off the campaign against salt, but most of the dire public health warnings are based on the Intersalt study, conducted in 1988, which measured average salt consumption and blood pressure levels in 52 groups randomly chosen from 32 countries. The study measured sodium intake against two things: the increase of blood pressure with age, and the median blood pressure of the group. The results overwhelmingly showed no particular correlation between salt intake and blood pressure: the graphs below, taken from INTERSALT’S conclusions, show the measured relationships between median blood pressure and sodium consumption.
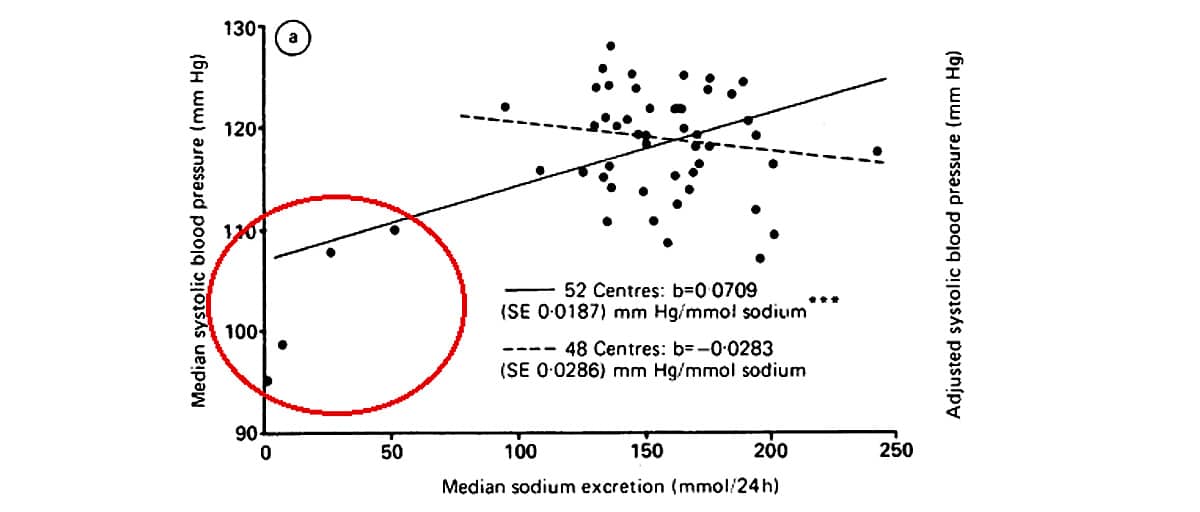
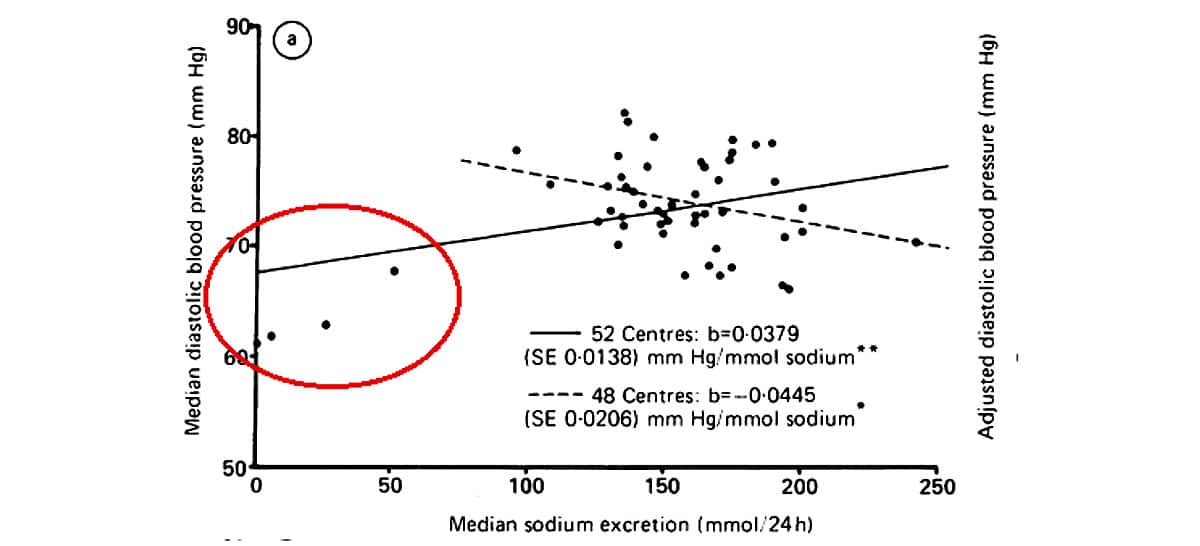
In each graph, notice that four data points (circled in red) are very far below the general cluster. According to the principles of scientific research, these data points are outliers, and ought to be excluded from the analysis. Outliers simply aren’t statistically significant, but they do skew the trend line. For example, if you drew a graph relating your consumption of spinach and the number of inches rained on any given day, chances are that on one or two days you would coincidentally eat very little spinach and observe very little rainfall. This doesn’t mean that your spinach consumption has any influence on the weather, but if you graphed your conclusions and drew a line through the data, these coincidental days would pull the end of the line down, showing a correlation that doesn’t actually exist.
This is what happened with the INTERSALT data. In the graphs shown, the solid lines are the trend lines when the outliers are included; the dotted lines show the observed trends with the outliers excluded. When the outliers don’t influence the trend lines, the correlation between salt intake and blood pressure disappears – even the Intersalt study itself admitted that without the four outliers, “both regression analyses showed no significant associations of sodium with median systolic pressure” (324). Like supporters of the theory that Paleolithic humans died young, however, advocates of salt restriction have manipulated the evidence by including the outliers.
These outliers are not only statistically insignificant, but also potentially indicative of factors completely unrelated to salt consumption. The Yanomami Indians, for example, were one of the groups represented by the outlier dots. They have very low salt intake, but they also have a relatively low BMI and almost no obesity or alcohol ingestion, low levels of dietary saturated fat, high levels of dietary fiber, a physically active lifestyle, and none of the chronic stressors of the modern lifestyle – all potentially confounding factors that could contribute to low blood pressure.
INTERSALT did appear to find a relationship between sodium intake and blood pressure increase with age, but other scientists have criticized this conclusion because it was not a hypothesis the study was designed to test, but rather an retroactive observation included because it proved what the researchers wanted to see. Also, without the outliers, even this relationship drops down to a “borderline level of significance” (322).
The Evidence Since INTERSALT

The inclusion of these outliers in the data set distorted the trend line, making the INTERSALT study appear to prove that salt restriction would lower blood pressure – a false correlation that only measured one potential effect of salt consumption. Despite the inadequacy of the data, the US government used it to set its official dietary recommendations. Based on this research, official NIH guidelines recommend no more than 2.4 grams of sodium a day for a healthy adult (equal to a little over a teaspoon of table salt). The American Heart Association goes even further, advising an upper limit of 1.5 grams a day.
These recommendations have spawned a rash of low-sodium products – canned soups, instant noodles, hot dogs, breakfast cereals, nut butters – most of which have very little relevance to anyone following Paleo in the first place (reduced-sodium ramen noodles aren’t any more Paleo than their ordinary counterparts). Even conventional medical wisdom is willing to acknowledge that “Fat in the diet doesn't make you fat!” as long as that dietary fat is replacing the new public health menace, sodium. But since the drive to reduce sodium consumption is based on such faulty data, the NIH recommendations beg the questions, is this preoccupation with dietary salt necessary? Could it even be harmful?
By1998, studies were increasingly finding fewer and fewer benefits of salt reduction, even at a public health level undetectable to individual subjects. In August of that year, Gary Taubes wrote an article summarizing the controversy and explaining why the link between salt and blood pressure (if it exists) is so difficult to determine. First of all, blood pressure is regulated by a complex homeostatic system: sodium affects it, but so do potassium, calcium, caloric intake, sex, age, and race. This introduces numerous complications to any study claiming that salt intake alone is responsible for high blood pressure.
Second, the early studies such as INTERSALT are all “ecologic” studies, comparing members of different populations (Yanomami Indians compared to Finns compared to Vietnamese compared to Americans). These studies appear to show that societies with a low salt intake have lower blood pressure, but they can’t account for the results of intrapopulation studies, which compare individuals within a certain population (white middle-aged men in Toronto). Within more homogenous population groups, researchers could find no direct relationship between dietary salt and higher blood pressure. Taking out the confounding factors that plague ecologic studies seemed to also reduce or eliminate the correlation between salt intake and blood pressure.
Further evidence that sodium is not directly responsible for high blood pressure arrived with the Dietary Approaches to Stop Hypertension (DASH) study in 1997. The DASH study held salt intake constant but found that a diet high in fruits, vegetables, and low-fat dairy produced a benefit for blood pressure much clearer than anything the salt restriction studies had been able to find.
In a more recent article in the New York Times, Taubes surveys the research since 1998. In 2001, the DASH-Sodium study seemed to prove that large reductions in salt intake would slightly lower blood pressure, but not necessarily result in any positive benefits like longer life or a lower risk of heart disease. The data from the DASH-Sodium study also showed that a DASH diet consistently outperformed a standard American diet, even at the same level of sodium intake, suggesting that sodium intake is far from the only dietary factor influencing blood pressure.
Not only does the evidence linking salt restriction to lower blood pressure seem increasingly inconclusive, but the corresponding assertion – higher blood pressure must be due to increased sodium intake – is also under fire. A study from 2003 found no significant change in dietary sodium levels since 1957. Despite dire public health warnings about the menace of sodium, American salt consumption has remained markedly stable: the recent rise in hypertension must therefore be attributable to some other cause. Another study from 2009 reached the same conclusion, and argued that humans naturally seek out a certain baseline level of sodium ingestion based on an inborn biological need that cannot be modified by governmental warnings.
This seems to show that sodium is particularly vital to the human diet: public health campaigns have successfully reduced consumption of fat, for example, but have so far had no similar effect on consumption of sodium. It might also indicate that sodium restriction, far from promoting health, could actually exacerbate the obesity epidemic. If sodium is such an important element of the diet that we evolved a failsafe method of getting enough of it, then reduced-sodium foods will simply prompt consumers to eat more of them in an attempt to meet their body’s sodium needs. Instead of eating 300 calories of ordinary bacon, they might need 500 calories of reduced-salt bacon to obtain the same amount of sodium.
The benefits of salt restriction and the capacity of public health officials to achieve that restriction, therefore, seem unclear at best. Lately, however, several studies have proven that long-term salt restriction not only does no measurable good, it can also be downright dangerous. Like glucose consumption, salt intake appears to show a U-shaped curve of benefits, with serious danger at the very low end and the very high end of the spectrum.
Especially for certain types of people, salt restriction can cause serious health problems very quickly. Athletes need salt to replace the electrolytes they lose through sweat – hence the salt in this Paleo "Gatorade" recipe. For Type 2 Diabetics, salt restriction can increase the risk of cardiac-related death and even for healthy people, a low-salt diet can promote insulin resistance. For the elderly, salt restriction can cause serious health problems, as it influences the body's response to other medications. Recent research, therefore, increasingly shows no significant benefit – and serious potential danger – from excessive salt restriction.
Salt and a Paleo Diet
While no studies have been done specifically tracking the effects of salt intake on Paleo, the research on the DASH diet provides valuable evidence. The DASH diet is not a perfect Paleo eating plan by any means (the sample menu advises dieters to “center your meal around carbohydrates”), but it does come much closer than the standard American diet. In both the 1997 and 2001 studies, the benefits commonly attributed to salt restriction (especially lower blood pressure) seemed to follow more from the diet itself, which emphasized fresh, whole foods with lots of fruits and vegetables. Something more complicated than salt intake was clearly influencing participants’ results in these studies – and that “something” was most likely the huge array of other vitamins, minerals, and micronutrients that influence blood pressure levels.
One of the most important of these nutrients was potassium. Potassium, which is found all kinds of fruits, vegetables, dairy products, and meats, seems to reduce the risk of hypertension – in a sense, it balances out any detrimental effects of sodium consumption. The ratio of sodium to potassium in the diet is particularly significant, especially for anyone interested in an evolutionary eating plan: one of the changes brought by the Agricultural Revolution was a drastic reversal of the ratio of dietary sodium to potassium. One NIH study even found that the ratio of sodium to potassium more strongly correlated with risk of cardiovascular disease than the absolute levels of sodium or potassium alone. Other studies found that the balance between the two elements is so important because a high ratio of sodium to potassium disturbs the body’s natural acid levels, slowing growth in children, and decreasing bone and muscle mass in adults, as well as contributing to the formation of kidney stones. The higher levels of potassium in the DASH diet probably produced much of the benefit to blood pressure levels.
Magnesium, another micronutrient available on the DASH diet but commonly deficient in the general population, also significantly reduced blood pressure in several studies. Other studies show that calcium may also have an effect. While these studies differ widely as to their findings about specific micronutrients and blood pressure, sodium is clearly not the only dietary factor at work.
This makes Paleo ideal from a blood pressure standpoint, since, like the DASH diet, it provides high doses of all the important nutrients that help maintain fluid homeostasis. The Paleo lifestyle also imitates several of the factors that made populations like the Yanomami Indians outliers in the INTERSALT study: low levels of stress, regular exercise, adequate sleep, and lowered intake of stimulants like caffeine.
In other words, without directly restricting salt, Paleo gets at the root causes of the lowered blood pressure touted by salt-reduction champions. This makes salt restriction itself not only unnecessary, but problematic. Human consumption of salt has shown a remarkable resistance to public health campaigns, suggesting that we’re physiologically designed for a certain level of salt intake and probably shouldn’t fight our bodies’ needs. Reviewing the available data suggests that a diet based on evolutionary science most closely meets human requirements for all of the many micronutrients regulating healthy blood pressure. Paleo might be naturally lower in salt than the standard American diet, due to the exclusion of sodium-rich processed foods, but there’s no need to artificially restrict sodium intake.
As well as worrying about the amount of salt they eat, many people wonder about the best kind of salt – pink Himalayan sea salt? Danish Viking-Smoked Sea Salt? Hiwa Kai Hawaiian Black Lava Salt? These specialty salts may have additional trace nutrients, and add an exciting flavor to your food; if you enjoy them, there’s certainly nothing harmful about them. They aren’t necessary, however: you can meet your sodium needs with ordinary table salt. The only danger of consuming sea salt is a potential iodine deficiency. While sea salt does contain other trace minerals, it does not have any iodine, as regular table salt does. If you choose to replace your table salt with sea salt, make sure to get enough iodine by eating kelp, seafood, or egg yolks, or by taking an iodine supplement.
Conclusion
Salt is not the enemy. Even though public health officials continue to scold us for enjoying it, their recommendations are based on faulty data and ignore the potential health problems of universal salt restriction. People with certain kidney problems may see some benefits from reducing salt consumption, but it’s not necessary or even healthy for most people. The historical stability of salt consumption suggests that our bodies know better than we do how much salt they need: on a Paleo diet rich in other important micronutrients like potassium, there’s nothing harmful about eating as much salt as you have a taste for.





Leave a Reply